as being a cause for many ailments, the primary one being osteoarthritis. However, as more research becomes available,
these claims are found to be increasingly baseless, showing that running at
reasonable volumes and intensities leaves the joint no worse for wear. And according to some studies, possibly better
than before!
What the research tells us:
 There are many studies suggesting that running is not detrimental
There are many studies suggesting that running is not detrimentalto the knees. In one such study, 504
former collegiate cross country runners were surveyed to assess their levels of
hip and knee osteoarthritis. The follow
up period for individuals was between two and fifty-five years, averaging
twenty-five years. Of those assessed,
only 2% reported severe pain, and only 0.8% had surgery for their
condition. They compared these results
to former collegiate swimmers, which had 2.4% reporting severe pain along with
2.1% having surgery (1). The evidence
from this study suggests that there is no association between moderate
long-distance running and the development of osteoarthritis. Additionally, it suggests that heavy mileage
and the number of years running are not contributory to the future development
of osteoarthritis.
athletes! How about when compared to
people who do not run regularly?
per week over 12 years) were compared to male nonrunners to assess a variety of
factors. The groups were compared in
perceived pain and swelling in the knees as well as the hips, ankles and
feet. Additionally, radiologic exams
were conducted to assess osteophytes (bony outgrowths in joints), cartilage
thickness, and overall grade of degradation.
There was no statistically significant difference between either group
for all measures, further suggesting that long-distance running is not
associated with premature join degradation (2, 5).
analyze the effects of physical activity on the individual structures of the
knee joint. After analyzing 1,362
studies, the data suggested that there is an association between physical
activity and osteophytes in the knee joint.
However, this is not necessarily a bad thing, and could possibly be an
adaptation to the stimuli associated with exercise. Additionally, the review states there is no
strong evidence on physical activity narrowing the joint space from cartilage
degradation. In fact, there is strong
evidence for an inverse relationship between physical activity and cartilage
defects (3). In other words, people who
are active have stronger cartilage in the knees than those who do not. This is further supported by a Swedish study,
in which researchers gave people at risk of osteoarthritis a running program,
and by the end showed improved biochemistry of the associated cartilages (5).
mean exercise time do not appear to increase the chances of developing
osteoarthritis in the knee. Despite
these findings, running is not an activity that everyone should participate in
without the proper guidance. Various
factors such as genetic predisposition, higher than average BMI, and previous
damage to the knee can all increase the chances of developing osteoarthritis
(4).
What you can do to prevent damage to your knees?
repetitive exercise can be a risk factor towards osteoarthritis (4), it is
important to try having a consistent, average BMI. Doing so will reduce the impact that your
feet and knees take. Did you know? Depending on the intensity, running can
create an impact of three to ten times a person’s body weight! (6)
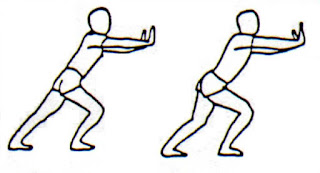
extremities. Research suggests that
running with a slightly forward-leaning trunk reduces stress on the
patellofemoral joint (7, 8), which is the part of the knee where the thigh bone
and knee cap meet.
rule”, in which during a training cycle weekly mileage does not increase by more
than 10% from week to week. The rule has
validity, with one 2014 study showing that runners who followed this rule were
less likely to become injured compared to a group that increased their mileage
by 30% (9).
In conclusion:
start and have no underlying knee issues, do not fear that running will damage
your knees. That being said, always talk
to a healthcare professional before making major lifestyle changes. Train smart, and above all, enjoy running!
Sohn, Roger S., and Lyle J. Micheli. “The Effect of Running on the Pathogenesis
of Osteoarthritis of the Hips and Knees.” Clinical Orthopaedics and Related
Research, no. 198, 1985
Panush, Richard S. “Is Running Associated With Degenerative Joint Disease?”
JAMA: The Journal of the American Medical Association, vol. 255, no. 9, 1986,
p. 1152.
Urquhart, Donna M., et al. “What Is the Effect of Physical Activity on the Knee
Joint? A Systematic Review.” Medicine & Science in Sports & Exercise,
vol. 43, no. 3, 2011, pp. 432–442.
Chakravarty, Eliza F., et al. “Long Distance Running and Knee Osteoarthritis.”
American Journal of Preventive Medicine, vol. 35, no. 2, 2008, pp. 133–138.
Neighmond, Patti. “Put Those Shoes On: Running Won’t Kill Your Knees.” NPR,
NPR, 28 Mar. 2011
Elert, Glenn. “Force on a Runner’s Foot.” E-World, 1999,
hypertextbook.com/facts/1999/SaraBirnbaum.shtml.
Teng, Hsiang-Ling, and Christopher M. Powers. “Sagittal Plane Trunk Posture
Influences Patellofemoral Joint Stress During Running.” Journal of Orthopaedic
& Sports Physical Therapy, vol. 44, no. 10, 2014, pp. 785–792.
Teng, Hsiang-Ling, and Christopher M. Powers. “Influence of Trunk Posture on
Lower Extremity Energetics during Running.” Medicine & Science in Sports
& Exercise, vol. 47, no. 3, 2015, pp. 625–630.
Nielsen, Rasmus Østergaard, et al. “Excessive Progression in Weekly Running
Distance and Risk of Running-Related Injuries: An Association Which Varies
According to Type of Injury.” Journal of Orthopaedic & Sports Physical
Therapy, vol. 44, no. 10, 2014, pp. 739–747.
post by Robbie Papapietro.